Treatment of Diabetic Retinopathy
Treatment of diabetic retinopathy by photocoagulation is of proven efficacy for both proliferative retinopathy and diabetic maculopathy. Transpupillary laser is applied so as to produce a retinal burn. Initially these burns appear as small fluffy areas similar to cotton wool spots...
Over time these may evolve into large pigmented scars similar in appearance to moon craters...
This was common with previous laser treatments; currently the power of the laser burns induces less damage to the retina and the appearance is less dramatic, commonly appearing greenish-grey...
Panretinal Photocoagulation, PRP
The rationale for treatment of new vessels (both at the disc and elsewhere) is that ablation of the peripheral retina reduces the overall oxygen damage of the eye. The ischaemic stimulus is therefore lessened and the new vessels can then regress.
The treatment produces a panretinal covering of non-confluent burns avoiding the macula. Treatment is usually delivered in two sessions, with the inferior half of the retina being treated first (since it is more likely to become inaccessible if a bleed occurs).
Destruction of the peripheral retina can be associated with constriction of the visual fields to such an extent that DVLC criteria for driving are no longer met. Other complications include:
Pain: This varies between individuals and in some cases retrobulbar anaesthesia is required.
Worsening macular oedema: This is usually a temporary phenomenon but maculopathy should ideally be treated before embarking upon PRP.
Focal laser therapy...
and grid laser therapy...
will reduce the risk of visual deterioration in patients with diabetic macular oedema by at least 50%. The strategy is to target areas of leakage (e.g. microanuerysms) using focal laser treatment and to use grid treatment for areas of diffuse leakage or capillary non-perfusion.
Note 1: Macular oedema cannot be diagnosed using the indirect ophthalmoscope and fluorescein angiography will be needed to pinpoint areas of capillary fall-out.
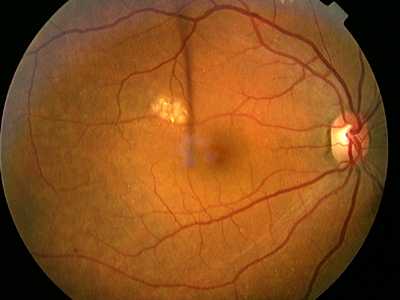
The image above shows areas of capillary fall-out particularly above the macula; these appear dark. The small white dots are retinal microaneurysms and dilated capillaries.
Note 2: Ischaemic maculopathy does not respond to laser treatment.
© 2000 Steve Bain, Jon Gibson, Paul Dodson, Graham Sedgwick