West Midlands Key Health Data 2009/10
CHAPTER SEVEN: CHANGES IN HEART ATTACK ADMISSIONS AND THE SMOKING BAN
Dr Khesh Sidhu: NHS West Midlands
Main Body
7: Changes in Heart Attack Admissions since the Smoking Ban
8: Measuring Disability Across the West Midlands
9: Surveillance of Clostridium Difficile in the West Midlands
7.1 Introduction
Over the last few years, there has been an increased focus on stop smoking services commissioned by PCTs. However, it is fair to say that there has been a wide variation in the numbers smokers attending these services over time and comparatively few smokers have used services as a proportion of the whole. A more dramatic change in societal behaviour took place in July 2007 when smoking was banned in enclosed places. This paper aims to examine trends in admissions for West Midlands patients admitted to hospital with heart attacks over the last 3 years.
7.2 Methods
Anonymised aggregate data was extracted to compare finished hospital stays (FHS – i.e. deaths and discharges) for patients that were assigned a Healthcare Resource Group (HRG) for a heart attack (Source WMCBSA). The time period spanned from April 2006 – November 2009 during which the Payment by Results (PbR) tariff relating to HRG rose. HRG codes changed in April 2009.
The HRG codes used in this analysis are;
- Acute Myocardial Infarction with or without complications and co-morbidities (used before April 2009)
- Actual or Suspected Myocardial Infarction (used after April 2009)
- Cardiac Arrest (used before and after April 2009)
Deaths in A&E, homes or care homes have been excluded. It has been assumed that most heart attack patients are generally sent to hospital for care and are quickly admitted to a hospital bed from A&E.
7.3 Results
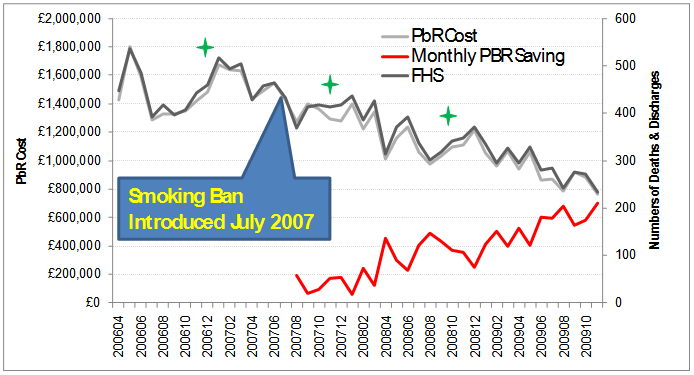
There has been a reduction in the numbers of FHS (deaths and discharges) associated with heart attacks over time (Figure 7.1). However scrutiny of Figure 7.1 not only shows that there was a change in the fluctuations over time, but the winter peaks of deaths were less marked. These are highlighted by the green stars in the figure below.
Figure 7.1: Deaths & Discharges for West Midlands Patients with Heart Attacks (West Midlands HES April 2006 – November 2009)
|
A more striking observation is that the PbR tariff costs have reduced (light grey line) and therefore cost savings have increased over time (red line).
PbR savings were calculated by comparing the monthly value for deaths & discharges after July 2007 with the average monthly value for the previous year (July 2006 – June 2007). It should be noted that PbR naturally rises because of tariff inflation.
Nevertheless, Figure 7.1 shows that there has been a halving of numbers of deaths and discharges since the smoking ban. As a result, it is therefore safe to infer that this has also been associated with a PbR saving of about half in a given year. This is the equivalent of c£6m per year. Differences in coding could account for some patients previously coded as heart attacks being coded as another HRG.
7.4 Are these trends significant?
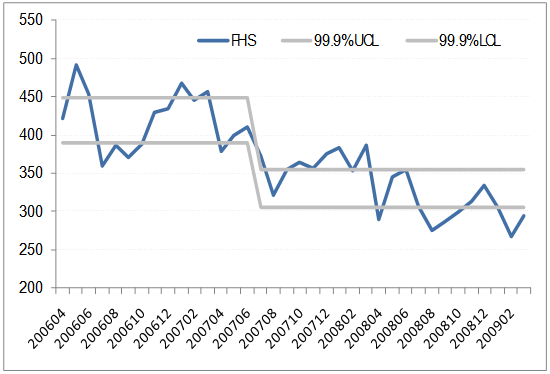
Figure 7.2 adds control limits to the time series by using 99.9% confidence limits (6Σ) to the charts. These were derived for the time frames as defined in Figure 7.2 and confirm a significant (99.9% CIs) step change after July 2007.
Figure 7.2: Deaths and Discharges for West Midland’s patients with Heart Attacks with Confidence limits. Year with month.
|
If data was available, the time series should extend before the time period as this reduction after July 2007 may have been part of a reducing trend in general.
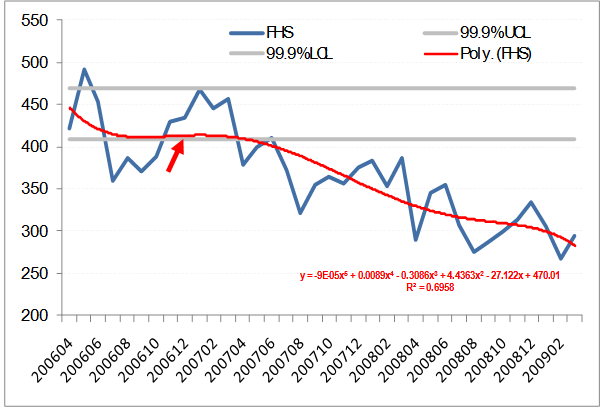
One way of adjusting for this is to add a trend line to observe changes in the slope. Figure 7.3 shows the polynomial trend line for the data and confirms a step change in the slope of the trend line in July 2007 (see red arrow).
Figure 7.3: Deaths and Discharges for West Midlands patients with Heart Attacks (polynomial trend line added) Year with Month
|
7.5 How are these affected by deprivation?
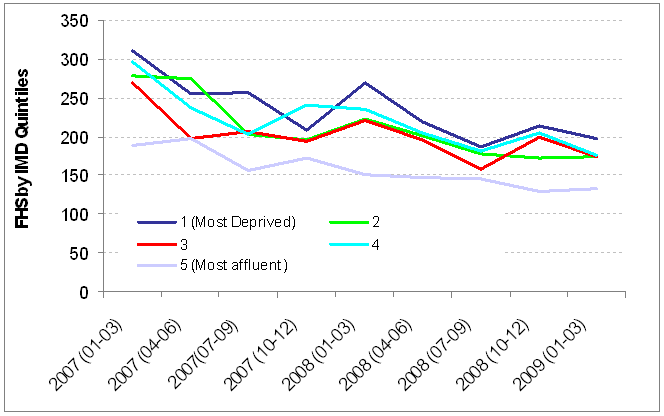
Heart disease and heart attacks are associated with more deprived populations due to a variety of reasons including lifestyle factors. Changes in lifestyle behaviour are known to occur disproportionately in the more affluent populations with ironically the lowest rates of heart disease. On this basis, a comparison of patients by IMD scores would be useful in understanding more about the impact of the smoking ban amongst different populations. Figure 7.4 dissects out the change in admissions over the time period by considering the 2007 IMD (Index of Multiple Deprivation) of each individual who was admitted with a heart attack during the time frame. The data presented previously was based on a monthly analysis. However, the figure below uses quarterly figures as the numbers of patients in different IMD groups are low. It is reassuring to note that Figure 7.4 shows a gentle reduction in the numbers of deaths in all IMD groups – including the most deprived populations – over the time period.
Figure 7.4: Deaths and Discharges for West Midlands patients with Heart Attacks (IMD 2007 added), Year (quarterly period)
|
7.6 Conclusions
There are some methodological areas that might be explored to further colour the conclusions drawn from the data. In particular, age standardised rates might be a better offering to ensure that fluxes in the populations attending have not resulted in a change in the numbers of heart attacks. Crude admission rates are unlikely to show any difference as the population of the West Midlands is so large that the marginal effect year on year would be indiscernible.
Access to earlier data prior to April 2006 would be useful to obtain as this would add further insights into long term trends. It is known that general long term trends for heart attack mortality have shown a steady reduction in the last 20 years.
Coding differences are bound to affect casemix. This ideally needs to be explored but with the advent of HRG4, it might be difficult to obtain like for like comparisons. Future work should focus on this.
The results are corroborated through further findings,
- published evidence from Scotland1 of reductions in heart attack related admissions post smoking ban
- published evidence that this reduced heart attacks amongst smokers and non-smokers2
- published evidence that there has been a measureable impact on second hand smoke inhalation3
- published evidence that the smoking ban was associated with changes in social-cognitive awareness as well as a reduction in number of cigarettes consumed4
- cardiologists have anecdotally noticed a reduction in the number of patients attending with heart attacks since the ban5
- recent reports confirm these findings with reductions in deaths1and admissions6
On balance, this chapter affirms the opportunities and apparent benefits for simple but cost effective public health interventions in reducing hospital admissions relating to tobacco smoking. There remain further opportunities in the “Stop before the Op” initiative.
References:
- Pell JP, Haw S. “The triumph of national smoke-free legislation.” Heart. 2009 Sep; 95(17):1377-9. Epub 2009 Jun 7.
- Pell JP ,Haw S, Cobbe S,Newby DE, Pell ACH, Fischbacher C, McConnachie A., Pringle S, Murdoch D, Dunn F, Oldroyd K, MacIntyre P, O'Rourke B and Borland W “Smoke-free Legislation and Hospitalizations for Acute Coronary Syndrome”, NEJM, Volume 359:482-491 July 31, 2008 Number 5
- Haw S and Gruer L “Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: national cross sectional survey”. BMJ 2007;335:549 published 9 September 2007.
- Orbell S, Lidierth P, Henderson CJ, Geeraert N, Uller C, Uskul AK, Kyriakaki M. “Social-cognitive beliefs, alcohol, and tobacco use: a prospective community study of change following a ban on smoking in public places”. Health Psychol. 2009 Nov;28(6):753-61.
- Personal communication with Dr D Connelly, Consultant Cardiologist, Sandwell and West Birmingham Hospital
- Sims M, Maxwell R, Bauld L and Gilmore A. “Short term impact of smoke-free legislation in England: retrospective analysis of hospital admissions for myocardial infarction” BMJ 2010; 340:2161.
Additional reference material
http://www.lho.org.uk/download.aspx?urlid=15261&urlt=1
For more information please contact Sarafina
Cotterill
© Public Health, Epidemiology and Biostatistics Unit, School of Health and Population Sciences, University of Birmingham